Easier Access to Health Data Is a Good Thing, Right?

On March 9, CMS and the Office of the National Coordinator for Health Information Technology (ONC) released the final versions of interoperability and information-blocking proposals they originally brought to the table last year. The consumer-focused rules overhaul how insurers, providers, and patients share health data, and are a new frontier for the U.S. healthcare system, says HHS Secretary Alex Azar.
The data rules come at a time when we have more computing power than ever coupled with a deep-seeded unhappiness with the state of American healthcare. On top of that, stakeholders are starting to point fingers at each other, suggesting greater accountability of all participants in the system—especially providers and payers.
What do patients think?
Patients care about data privacy and personalization. In a survey of 2,200 patients conducted by Morning Consult on behalf of AHIP, the national trade association for America’s health insurance companies, the consensus was that privacy protection outweighs the ease of access to health information.
CMS originally provided a cost estimate of $718,000 – $2.3 million per payer, leading them to believe that they would need to raise premiums to compensate. Notably, three in four respondents would not support any regulations that made it easier to find the cost of medical procedures if it meant raising the cost of premiums.
Over 80% of respondents believe that when searching for information about a medical service, it should be focused but easy to understand instead of comprehensive yet confusing. This presents communication challenges that providers and insurers would need to consider when they think about what information to present. What’s more, two in three patients said they wanted to access personalized information about their insurance, meaning communication would need to take into consideration factors like the individual, location, type of coverage, and the appropriate level of detail to convey.
The Data Rules
Aimed at providing better access to quality-driven providers, the rules are significant because they:
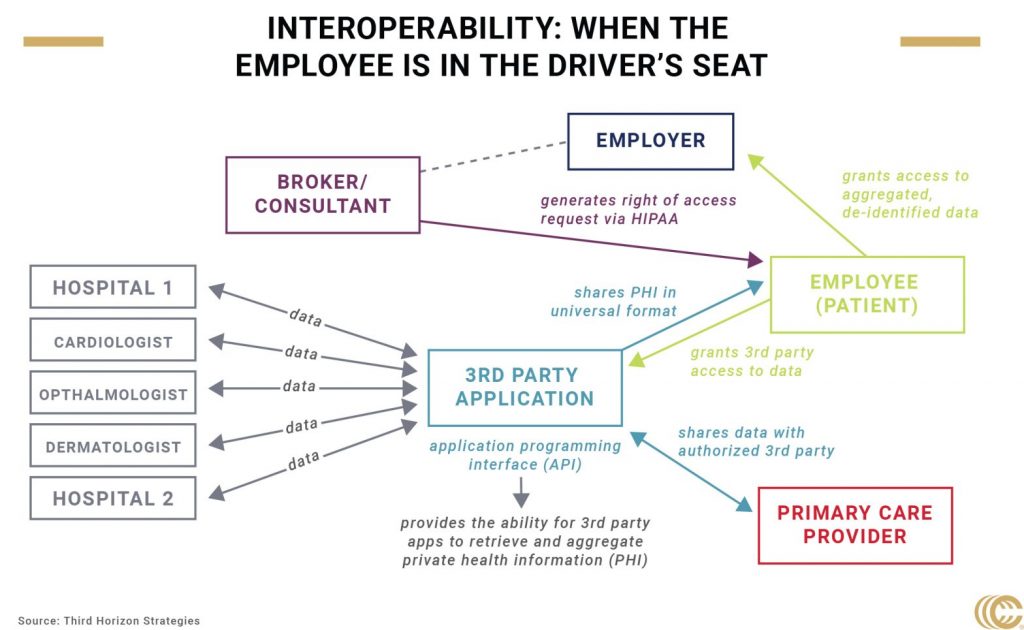
- Outline “bulk” requirements for payers and providers. Data-sharing capabilities are extended beyond individual consumer use cases to bulk access for population level datasets. In these situations, payers receive clinical data in order to assess care quality, and claims data to access the type of care patients get in and out of the network. This could allow employers to pool data together to glean insights, a potential key for population health management.
An example in practice: CMS launched an Accountable Care Organization (ACO) Beneficiary Claims Data pilot to receive claims data and standardize it. Value-based payments use hospital-specific metrics to measure performance and are used for remediation or the following year’s contract.
- Provide consumers access to “all data elements” instead of limited elements of their health records, creating the opportunity for better care coordination patients to develop a longitudinal health record combining multiple portals and providers over time.
Why this is important today: Doctors often provide care using an incomplete clinical picture. That could be especially problematic during a pandemic, when the healthcare system will be stressed and when patients are more-or-less at risk depending on pre-existing conditions and their medical history.
- Balance privacy and consumers’ right of access. CMS and ONC allow payers and providers to communicate warnings about suspected apps that fail to abide by certain privacy codes of conduct. That enables stakeholders to police each other and creates a direct line of communication between payers, providers, and consumers.
Why this is easier said than done: Consumers have privacy concerns that outweigh their desire to easily access their health information. The challenge will be demonstrating to patients that their data is secure, but the message will need to be consistent across payers, providers, and employers.
Where Employers Can Play a Role
- Demand: The rule does not apply to commercial payers, but they will have the capability to implement the rules into commercial plans due to the Medicare Advantage plans they administer. The opportunity for brokers and employers here would be to create demand around this functionality for the employer-sponsored market. That demand could emphasize new underwriting, risk assessment, and population health management capabilities enabled by access to patient data, while at the same time communicating privacy concerns and representing the interests of employees.
- Personalization: Self-insured employers have flexibility in how they cover their employees. That flexibility leads to the need to customize the information presented to patients about their coverage and treatment options as well as their health data.
- Education: Employers could also spearhead employee education efforts, syncing plan information, privacy requirements, and driving employees to use particular vetted applications to retrieve and share their health data.
These data interoperability rules emphasize the role and responsibility of the healthcare consumer at a time when the care delivery system will be strained by COVID-19. Some provider groups have argued that work to implement these new rules would draw necessary resources away from responding to the global pandemic. However, others argue that the need to open up the flow of data, given the emphasis on telemedicine and lab testing, is greater than ever before. We’ll continue to watch these dynamics and how they’ll intersect with the development of new privacy laws and other employer-led efforts targeting consumers.